
[ad_1]
Having played professional rugby for almost 20 years, former British Lions captain Alun Wyn Jones was used to pushing his body hard, so when three years ago he started to become occasionally breathless and felt as if his heart was racing, he just shrugged it off.
‘You can get a fast heart rate after having caffeine, so I thought it might be due to a strong cup of coffee,’ says Alun, 39, who lives near Swansea with his wife Anwen, a university lecturer, and their three daughters.
And Alun rationalised that, as ‘about 90 per cent of my time was spent running around’, being out of puff after a match was to be expected, even for him, the world’s most capped international rugby union player with 158 appearances for Wales.
However, medical checks he underwent before signing for a new team in southern France last year revealed his optimism was misguided.
To Alun’s horror, the checks found he had a serious heart complaint – atrial fibrillation or AF, meaning his heart beats erratically, putting him at a significantly increased risk of a stroke.

After medical checks, Alun Wyn Jones found he had a serious heart complaint – atrial fibrillation or AF, meaning his heart beats erratically, putting him at an increased risk of stroke
The condition affects around 1.4 million in the UK – and cases are on the rise, even among fit, relatively young people.
While the diagnosis was ‘a massive shock,’ Alun says it also ‘actually came as a bit of a relief’. ‘It joined up all the dots – for about 18 months to two years before my diagnosis I’d felt tiredness and wondered if I had chronic fatigue.
‘My sleep was being disrupted and I had these fleeting palpitations in my chest and felt a bit breathless. But my symptoms were so innocuous I dismissed them.’
Indeed it’s the innocuous nature of the symptoms – which also include light-headedness – that means so many cases go undiagnosed; almost 300,000 people live with AF without knowing they have it, according to the British Heart Foundation. This is a concern, as the condition puts them at a five times greater risk of a stroke.
In AF, which is the most common heart rhythm disorder, the heart beats erratically and sometimes also faster or slower than normal (usual heart rate is between 60-100 beats per minute, but in AF it can be as high as 200).
The condition is caused by abnormal electrical activity in the top chambers of the heart (the atria) – as a result, these don’t fully contract, so they’re out of synch with the two lower chambers. While it’s not on its own life-threatening, AF makes blood clots more likely and these can travel to the brain, blocking blood flow resulting in a stroke.
And the number of AF cases has risen dramatically, says Andre Ng, a consultant cardiologist at Glenfield Hospital in Leicester and a professor of cardiac electrophysiology at the University of Leicester.
‘About 10-15 years ago we used to say it affects 1-2 per cent of the population, but now it’s around 2-3 per cent,’ he says.
‘One of the driving forces for this is that we’re living longer – one in ten people over 70 has AF – and as we get older we have more time to acquire other conditions that can trigger AF, such as diabetes, high blood pressure, heart disease and heart failure.’

Having played professional rugby for almost 20 years, the former British Lions captain was used to pushing his body hard
Another driver in people of all ages is obesity – which may lead to inflammation in the heart tissue. ‘But I also see a lot of younger, sporty people in my practice who have AF,’ he adds.
A review in the British Journal of Sports Medicine in 2021 found that people under the age of 55 who did regular ‘endurance and mixed sports activities’ were almost two-and-a-half times more at risk of AF than non-athletes.
‘We know exercise is good,’ says Professor Ng, ‘but too much exercise is not necessarily good for us – and excessive exercise, for instance at a particularly competitive level and prolonged endurance training, may cause additional stress on the heart.’
That’s because it pushes your blood pressure up, ‘so the heart is under stress’, says Professor Ng.
‘If you do that repetitively, the extra stress may ‘stretch’ cells in the heart and cause them to be excited and ‘fire’ electrically, causing extra beats in the heart that trigger AF. I see quite a lot of enthusiastic or competitive athletes, especially long-distance runners, who have atrial fibrillation early on in their career.’
One reason more cases are being picked up among younger people is the growing use of ‘smart’ watches, some of which can detect potential heart rhythm problems, he says. AF is diagnosed with an electrocardiogram (ECG) which records the heart’s electrical activity via small sensors attached to various points on the chest and body.
Alun had a normal ECG in 2021 – but the one he then had last July as part of his medical checks before joining French rugby club Toulon ‘showed up straight away something wasn’t right’, he says. The doctor explained there and then that he had AF but he was lucky it was spotted – as it may not be detectable all the time.
Professor Ng says once AF is diagnosed then any underlying cause, such as high blood pressure, which increases the AF risk as it stresses the heart, will be treated. Treating the cause can help better control AF symptoms. ‘If there isn’t an underlying cause, we try to reduce the long-term effects of AF, which are the risk of stroke and heart failure,’ he adds.
AF that comes and goes – called paroxysmal AF – may be treated with drugs such as beta blockers that slow the heart rhythm or blood thinners to prevent clots. Patients with more persistent AF may be offered cardioversion – where an electric shock is applied to ‘reset’ the heart rhythm.
An alternative is catheter ablation, where a thin, flexible tube is passed through a blood vessel in the groin to the heart and the area producing the faulty rhythm is destroyed using heat or freezing.
This causes a scar in the heart that the abnormal electrical activity cannot pass through. Alun was advised that cardioversion was best for him, as his symptoms were persistent.
‘I knew I would have my treatment once I’d finished my short-term contract, so went out and played, focusing on the games,’ says Alun, who joined Toulon from Swansea-based Ospreys in July 2023. ‘I carried on as normal but was more aware of my body.’
Alun played his last professional game last November: two weeks later he had the cardioversion. ‘It was just like getting plugged into the socket I was told by the medical team,’ says Alun.
‘After the cardioversion, the symptoms – the palpitations and shortness of breath – stopped, and I was no longer so fatigued.’
Today, he doesn’t take medication but uses a KardiaMobile heart monitor, which has pads you place your fingers on to record the heart’s electrical activity in 30 seconds. The results are then sent to an app on your mobile phone.
‘This piece of kit gave me peace of mind,’ he says. ‘If I felt a palpitation and wondered is that indigestion or too much caffeine, I might get it out and use it.’
He keeps fit, for example, by swimming, running and cycling, and remains grateful he had the medical with Toulon.
‘I’d have finished my playing career and never known about my atrial fibrillation, which would probably have put me in a worse position sometime in the future,’ he says. ‘By diagnosing it when they did, it’s a good thing for me, and I’m now making others aware of it, too.’
Alun is working with AliveCor’s Let’s Talk Rhythm campaign to raise awareness about atrial fibrillation.
Vitamin maths
‘Vitamin B12 helps create red and white blood cells and platelets [important for blood clotting], and DNA,’ says dietitian Frankie Phillips. ‘B12 also helps keep hair, nails and skin healthy.
We get it from foods of animal origin – good sources include meat, fish, poultry, milk, eggs, fortified breakfast cereals and plant milks and nutritional yeasts.’ Vegans may need to take a B12 supplement.
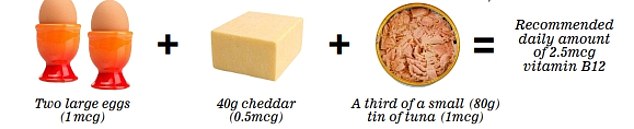
The foods that add up to your recommended daily nutrient intake
[ad_2]
Copyright for syndicated content belongs to the linked Source link

